This post is available in:
![]() Dansk
Dansk
Version 1.20, København, den 9.11.2020: 1 tilføjelse
Version 1.10, København, den 3.10.2020: 1 tilføjelse
Version 1.00, København, den 1.10.2020
Jeg har allerede skrevet et par tekster om D vitamin på mit website, f.eks. teksten Vitaminer og mineraler kan afskaffe COVID-19 epidemien, hvoraf det fremgår at hvis man har over 75 nmol D vitamin pr. liter blod er det næsten umuligt at blive alvorligt syg af ’COVID-19’. Dette blev understøttet af et par videnskabelige artikler. Jeg sendte også teksten til alle Folketingets medlemmer, men det interesserede dem ikke…
Nu har en ven så fundet 49 videnskabelige artikler som bekræfter D vitamins positive effekt mod bl.a. covid-19 og andre infektioner og meget andet.
Til sidst i nedenstående liste er der et kort email fra læge Claus Hancke, som er rasende over at DR (igen) manipulerer for at underspille hvor vigtige vitaminer er for vores helbred…
KH
Henrik
| Tilføjelse i version 1.10, den 3.10.2020: |
|---|
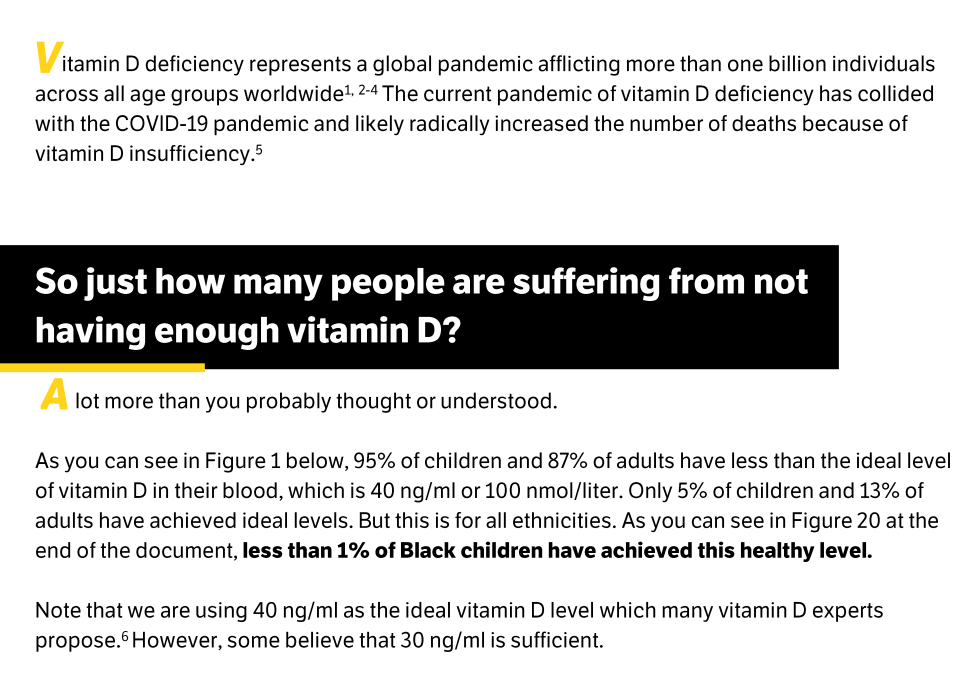
134 videnskabelige artikler om D vitamin og COVID-19 osv.!Jeg er ret overvældet. Dr. Mercola og 4 andre læger har lavet 2 versioner af en længere rapport om hvor vigtigt D vitamin er i forhold til COVID-19 mv.! Se https://www.stopcovidcold.com/ Den lange version har en liste med 185 kilder(!) hvoraf de 134 handler om D vitamin! Det er lidt vildt! Her er starten af rapporten (man kan ikke kopiere tekst fra den, kun i kildelisten):
Men de skriver også:
KH |
| Tilføjelse i version 1.20, den 9.11.2020: |
|---|
Den korte version af ovennævnte rapport fra Dr. Mercola og 4 andre læger indeholder det følgende kapitel:
Other Nutrients That May Increase the Effectiveness of Vitamin D SupplementationSince over half the population does not get enough magnesium, and far more are likely deficient, magnesium supplementation is recommended when taking vitamin D supplements. This is because magnesium helps to activate vitamin D, as the enzymes that metabolize vitamin D in the liver and kidneys require magnesium. In fact, about half of those taking vitamin D supplements are unable to normalize their vitamin D levels until they take magnesium. GrassrootsHealth found that those who do not take supplemental magnesium need, on average, 146% more vitamin D to achieve a blood level of 40 ng/ml (100 nmol/L), compared to those who take at least 400 mg of magnesium per day. The dose of magnesium should be around 500 mg/day, but more if you don’t have the loose stools that can occur with higher-dose magnesium supplementation. If you have kidney damage, discuss the dose with your physician. Take at least 500 mg of magnesium with your vitamin D One can also take 150 to 200 mcg of vitamin K2 per day, as it works synergistically with vitamin D. This will help drive the calcium that vitamin D helps increase in your blood, and drive it into your bones to build healthier bones. The only concern is that if you are on Coumadin, you have to discuss vitamin K2 with your physician as it will interfere with Coumadin. |
———————————–
Fra Mads Wedel-Ibsen
Formand / Chairman / Präzident
May Day Danmark
– oplysningsforbundet til fremme af selvansvar og sundhedsbevidsthed
– The Civil Health Rights Movement May Day
– Verein zur Information und für Förderung von Gesundheit und Selbstbestimmung

Jeg har samlet lidt D vitamin-evidens her… Primært om infektioner og sol:
This study is the first to document a statistically significant correlation between a country’s latitude and its COVID-19 mortality and is consistent with other research regarding latitude, Vitamin D deficiency, and COVID-19 fatalities.
https://pubmed.ncbi.nlm.nih.gov/32599103/
Based on literature review, we highlight the findings regarding the protective role of vitamin D for infectious diseases of the respiratory system.
https://pubmed.ncbi.nlm.nih.gov/32491112/
Accumulating evidence suggests that 1,25-dihydroxyvitamin D3 exerts protective effects during infections by upregulating the expression of cathelicidin and β-defensin 2 in phagocytes and epithelial cells. Vitamin D may be acting as a panaceal antibiotic agent and thus may be useful as an adjuvant therapy in diverse infections.
https://pubmed.ncbi.nlm.nih.gov/24593793/
High-dose vitamin D (1200 IU) is suitable for the prevention of seasonal influenza as evidenced by rapid relief from symptoms, rapid decrease in viral loads and disease recovery. In addition, high-dose vitamin D is probably safe for infants.
https://journals.lww.com/pidj/Fulltext/2018/08000/Preventive_Effects_of_Vitamin_D_on_Seasonal.5.aspx
Epidemiologic evidence links vitamin D deficiency to autoimmune disease, cancer, cardiovascular disease, depression, dementia, infectious diseases, musculoskeletal decline, and more.
https://pubmed.ncbi.nlm.nih.gov/22461123/
vitamin D deficiency has been linked to increased risk for preeclampsia, requiring a cesarean section for birthing, multiple sclerosis, rheumatoid arthritis, types I and II diabetes, heart disease, dementia, deadly cancers, and infectious diseases.
https://jim.bmj.com/content/59/6/872
Vitamin D supplementation was safe and it protected against acute respiratory tract infection overall. Patients who were very vitamin D deficient and those not receiving bolus doses experienced the most benefit.
https://www.bmj.com/content/356/bmj.i6583
Insufficiency and deficiency of 25-hydroxyvitamin D and reduced exposure to sunlight were significantly associated with an increased risk of Parkinson’s disease.
https://pubmed.ncbi.nlm.nih.gov/30672512/
This study’s findings showed that sunlight exposure was associated with recovery from Covid-19.
https://www.sciencedirect.com/science/article/pii/S004896972032533X
The evidence for an association between vitamin D and risk of influenza infection exists, albeit mainly in in vitro and animal studies describing the role of 1,25(OH)D in innate and adaptive immunity. Observational human studies of 25(OH)D deficiency and randomized controlled trials supplementing various forms of vitamin D have yielded mixed but promising results.
https://academic.oup.com/advances/article/3/4/517/4591501
Clinically, there is evidence of the association of vitamin D insufficiency and respiratory tract infections. There is also some evidence of the prevention of infections by vitamin D supplementation. Randomised controlled trials are warranted to explore this preventive effect.
https://pubmed.ncbi.nlm.nih.gov/22115013/
Vitamin D is essential for good health, especially bone and muscle health. Many people have low blood levels of vitamin D, especially in winter or if confined indoors, because summer sunshine is the main source of vitamin D for most people
https://nutrition.bmj.com/content/early/2020/06/10/bmjnph-2020-000089
Evidence supporting the role of vitamin D in reducing risk of COVID-19 includes that the outbreak occurred in winter, a time when 25-hydroxyvitamin D (25(OH)D) concentrations are lowest; that the number of cases in the Southern Hemisphere near the end of summer are low; that vitamin D deficiency has been found to contribute to acute respiratory distress syndrome; and that case-fatality rates increase with age and with chronic disease comorbidity, both of which are associated with lower 25(OH)D concentration.
https://pubmed.ncbi.nlm.nih.gov/32252338/
In conclusion, we found significant crude relationships between vitamin D levels and the number COVID-19 cases and especially the mortality caused by this infection. The most vulnerable group of population for COVID-19, the aging population, is also the one that has the most deficit Vitamin D levels.
https://link.springer.com/article/10.1007/s40520-020-01570-8
Study confirms vitamin D protects against colds and flu”
https://news.harvard.edu/gazette/story/2017/02/study-confirms-vitamin-d-protects-against-cold-and-flu/
This study suggests that vitamin D supplementation during the winter may reduce the incidence of influenza A, especially in specific subgroups of schoolchildren
https://academic.oup.com/ajcn/article/91/5/1255/4597253
According to Grant and Giovanucci [48], vitamin D supplements or fortified foods should be evaluated further as a possibly useful component of a programme to reduce influenza mortality rates, especially in elderly persons.
The studies clearly show that vitamin D is, undoubtedly, part of the complex factors which affect the immune response.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6121423/
To reduce the risk of infection, it is recommended that people at risk of influenza and/or COVID-19 consider taking 10,000 IU/d of vitamin D for a few weeks to rapidly raise 25(OH)D concentrations, followed by 5000 IU/d. The goal should be to raise 25(OH)D concentrations above 40–60 ng/mL (100–150 nmol/L). For treatment of people who become infected with COVID-19, higher vitamin D doses might be useful.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7231123/
In the randomized trials and meta-analysis, vitamin D supplementation has been shown to have protective effects against respiratory tract infections; therefore, people who are at higher risk of vitamin D deficiency during this global pandemic should consider taking vitamin D supplements to maintain the circulating 25(OH)D in the optimal levels (75–125 nmol/L).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7305922/
Influenza infection remains a major public health concern across the world. The overall body of evidence suggests that older adults are more prone to be infected by influenza virus. While influenza prevention strategies are mainly based on immunization, current influenza vaccines do not offer optimal protection in this population due, in part, to waning immunity. Even if VitD has profound effects on immunity and clinical and epidemiological data suggest that VitD insufficiency increases susceptibility to influenza infection, there is not yet sufficient information to clarify the true relationship between VitD status and host resistance or influenza vaccine immunogenicity.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3228300/
In this sample of the general Danish population, not including at-risk groups but encompassing children and adults between 2 and 69 years old, we found substantial seasonal variation in the 25(OH)D concentrations. Most participants were vitamin D-sufficient in autumn, but many experienced vitamin D insufficiency during the spring, emphasizing the need for individual, bi-seasonal measurements when assessing status.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6265892/
In conclusion, we found significant crude relationships between vitamin D levels and the number COVID-19 cases and especially the mortality caused by this infection. The most vulnerable group of population for COVID-19, the aging population, is also the one that has the most deficit Vitamin D levels.
Vitamin D has already been shown to protect against acute respiratory infections and it was shown to be safe. It should be advisable to perform dedicated studies about vitamin D levels in COVID-19 patients with different degrees of disease severity.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7202265/
Aggregated evidence from 11 randomized controlled trials indicates that supplementation with vitamin D could be an effective means of preventing respiratory tract infection.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3686844/
Vitamin D with calcium reduces mortality in the elderly, whereas available data do not support an effect of vitamin D alone.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3410276/
In summary, there is possible evidence from RCTs for protective vitamin D effects on TB and likely evidence for protective effects on acute airway infection. Since vitamin D deficiency is prevalent in Europe, especially in institutionalised individuals and non-European immigrants, daily oral vitamin D intake, e.g. 1000 international units, is an inexpensive measure to ensure adequate vitamin D status in individuals at risk.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4806418/
The high prevalence of vitamin D insufficiency is a particularly important public health issue because hypovitaminosis D is an independent risk factor for total mortality in the general population.[
Emerging research supports the possible role of vitamin D against cancer, heart disease, fractures and falls, autoimmune diseases, influenza, type-2 diabetes, and depression. Many health care providers have increased their recommendations for vitamin D supplementation to at least 1000 IU.[] A meta-analysis published in 2007 showed that vitamin D supplementation was associated with significantly reduced mortality.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3356951/
vitamin D, vitamin C, zinc, and Echinacea have pivotal roles of three main immunoreactive clusters (physical barriers, innate and adaptive immunity) in terms of prevention and treatment (shortening the duration and/or lessening the severity of symptoms) of common colds. The present narrative review demonstrated that current evidence of efficacy for zinc, vitamins D and C, and Echinacea is quite strong that CC patients may be encouraged to try them for preventing/treating their colds.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5949172/
Dearth of treatment for COVID-19 leaves us with no choice but to take precautionary and prophylactic measures to stand a better chance to fight this pandemic. Hence, maintaining adequate Vit D levels is vital to prevent getting infected or to ward off the infection without mortality, in case it occurs. Clinical trials should be conducted in regard to COVID-19 for assessing the effect of Vit D supplementation and determining the appropriate dose. We conclude that correlation exists between Vit D levels and COVID-19 susceptibility and Vit D could prove to be an essential element in our fight against COVID-19.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7266578/
Evidence is presented suggesting a direct correlation between sunlight exposure and reduced mortality.
This study is the first to document a statistically significant correlation between a country’s latitude and its COVID-19 mortality and is consistent with other research regarding latitude, Vitamin D deficiency, and COVID-19 fatalities. Limitations of this study are noted.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7319635/
While oral sources of vitamin D could be used instead of UVB or when UVB irradiance is not available, public health policies do not yet recommend the 3,000–4,000 IU/day required to raise serum 25-hydroxyvitamin D levels to the levels required for optimal health, which would be required before vitamin D fortification levels in food can be raised. Until then, moderate solar UVB irradiance remains an import source, and the health benefits greatly outweigh the risks.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2835876/
The data support the hypothesis that a high vitamin D level, as that found in the summer, acts in a protective manner with respect to influenza as well as pneumonia.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3092571/
School children in Japan who received 1200 IUs of vitamin D daily for 4 mo during the winter reduced their risk of developing influenza infection by 42%.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3897598/
There is potentially a great upside to increasing the vitamin D status of children and adults worldwide for improving musculoskeletal health and reducing the risk of chronic illnesses, including some cancers, autoimmune diseases, infectious diseases, type 2 diabetes mellitus, neurocognitive disorders, and mortality.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3761874/
Vitamin D also reduces the production of proinflammatory cytokines, which could also explain some of the benefit of vitamin D since H1N1 infection gives rise to a cytokine storm. The potential role of vitamin D status in reducing secondary bacterial infections and loss of life in pandemic influence requires further evaluation.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2835877/
There is ample evidence that various non-communicable diseases (hypertension, diabetes, CVD, metabolic syndrome) are associated with low vitamin D plasma levels. These comorbidities, together with the often concomitant vitamin D deficiency, increase the risk of severe COVID-19 events. Much more attention should be paid to the importance of vitamin D status for the development and course of the disease. Particularly in the methods used to control the pandemic (lockdown), the skin’s natural vitamin D synthesis is reduced when people have few opportunities to be exposed to the sun.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7276229/
Ultraviolet radiation (either from artificial sources or from sunlight) reduces the incidence of viral respiratory infections, as does cod liver oil (which contains vitamin D).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2870528/
Most studies agree in that decreased vitamin D concentrations are prevalent among most infants and children with RTIs. Also, normal to high-serum 25(OH)D appears to have some beneficial influence on the incidence and severity of some, but not all, types of these infections.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7092025/
A new meta-analysis confirmed that low 25(OH)D levels were associated with a significant increased risk for all-cause mortality.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4377887/
Obese children and adults and children and adults on medications such as anticonvulsants, glucocorticoids or AIDS medications need at least two to three times more vitamin D for their age group to satisfy their body’s vitamin D requirement.
The results of these studies are consistent with the recommendation to improve the general vitamin D status in children and adults by means of a healthy approach to sunlight exposure, consumption of foods containing vitamin D and supplementation with vitamin D preparations.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4377887/
The epidemiological features of septicemia, including seasonality, racial disparity, increased rate with age, and several clinically significant comorbidities, are similar to the epidemiology of vitamin D deficiency. The hypothesis that higher levels of 25(OH)D reduces the incidence and improve the prognosis of septicemia should be easy to test.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2715199/
As a conclusion, in this period when we fought against the COVID-19 pandemic, which affected many countries around the world and caused thousands of people to die, no clear agent has been found in its treatment. In fact, an easily accessible agent such as vitamin D may be an important weapon in our hands. However, there is no clear evidence for high-dose or dose of vitamin D supplementation in patients with SARS-CoV-2 infection.
Although there is a need for more research related to this subject, we think that supplementing vitamin D as a part of standard nutrition may be somewhat effective in providing clinical benefit.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7293167/
Although the health benefits of vitamin D sufficiency are clear, awareness of the dangers of vitamin D deficiency is lacking. People with vitamin D deficiency have no obvious symptoms until it is so severe that they develop osteomalacia; this is often misdiagnosed as fibromyalgia, so many doctors may not be aware of the problem. Public health campaigns that emphasise the insidious consequences of vitamin D deficiency on health are therefore needed. Regulatory health agencies also need to provide recommendations for sensible sun exposure, especially for ethnic minorities. They should also implement aggressive fortification of foods—supplementation should be increased from 100 IU per serving to at least 200 IU. The US, Canada, Sweden, and Finland already fortify milk with vitamin D but this policy should be extended to Europe. More foods, such as pasta, other dairy products, and orange juice should be fortified.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2427138/
There are now several thousand publications that support the non-skeletal health benefits of vitamin D that should not be ignored either because they are association studies or small randomized controlled trials. There is no evidence that there is a downside to increasing vitamin D intake in children and adults with the exception of those with chronic granuloma forming disorder or lymphoma. It will take several more years to hear from several ongoing large RCTs evaluating non-skeletal benefits of vitamin D. If you believed and followed the IOM recommendation of 200 IU/d in 1997 then for the past decade you were likely vitamin D deficient. 600 IU/d that the IOM now recommends will raise and maintain blood concentrations of 25(OH)D > 20 ng/ml but < 30 ng/ml. Based on the overwhelming cumulative reports this is not satisfactory to obtain all of the health benefits of vitamin D. The evidence-based recommendations by the Endocrine Society’s Clinical Practice Guidelines are more realistic (400–1,000 IU for children, 1,500–2,000 IU for adults to maintain 25(OH)D concentrations of 40–60 ng/ml for preventing and treating vitamin D deficiency.46
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3427198/
The current policy of sun avoidance is creating probable harm for the general population.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4536937/
Vitamin D deficiency is a common, serious medical condition that significantly affects the health and well-being of older adults.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4399494/
Though some prospective studies show positive results regarding vitamin D on infectious disease, several robust studies are negative. Factors such as high variability between studies, the difference in individual responsiveness to vitamin D, and study designs that do not primarily investigate infectious outcomes may mask the effects of vitamin D on infections.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4346469/
The second question was why we did not point out that African Americans (AAs) have a much higher risk of COVID-19 infection and death than white Americans. At the time we submitted our manuscript, the data comparing AA COVID-19 infection and mortality rates were not available. In addition, there are a number of other reasons why AAs have higher COVID-19 rates, including that they have higher chronic disease rates than white Americans [24]. People with chronic diseases generally have low 25(OH)D concentrations (see Table 2 in [2]). Now, however, it is well-known that AAs have much higher COVID-19 infection and mortality rates [25]. Based on the National Health and Nutrition Examination Survey (NHANES) 2001–2010, the prevalence of serum 25(OH)D concentrations <20 ng/mL was 72% for non-Hispanic blacks (NHBs), 43% for Hispanics, and 19% for non-Hispanic whites, with the prevalence of <10 ng/mL being 17% in NHBs [26]. Of all the risk factors AAs have for becoming infected with COVID-19, raising serum 25(OH)D concentrations is the easiest one to counter”.
Vitamin D Supplementation in Influenza and COVID-19 Infections
Inadequate amounts of vitamin D in older people reduces well being, aggravates the ageing process, in particular reducing mobility and adds to the severity of osteoporosis and the risks of falls and fragility fractures with all of their severe consequences. It also reduces longevity, increasing the risk of cardiovascular deaths in particular, but may also increase the risks of type 2 diabetes and certain common cancers, notably colo-rectal cancer.
Since adequate exposure to summer sunshine becomes increasingly difficult for everyone with modern lifestyles, and more so with age, maintaining good intakes of vitamin D throughout life and increasing the amount taken in those aged 60–70 years or more would ensure that the problems that hypovitaminosis D aggravates with ageing are minimized.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3501367/
Fra: Claus Hancke
Sendt: 10. september 2020 14:58
Emne: DR manipulerer groft
Kære venner
Hvis I vil hidses op i det røde felt, så se (eller optag) “Vitaminpiller – myte eller mirakelkur?” Den genudsendes på DR2 kl: 01.00 i nat.
Jeg så den forleden.
Det er en himmelråbende manipulerende udsendelse fra BBC proppet med fordrejninger og faktuelle fejl og derefter oversukret med en klovnet fremstilling. (Jaja. Gluud er også med)
DR gør sig her skyldig i ensidig og stærkt manipulerende journalistik, -uden modsvar.
Det var aldrig sket, hvis det var en positiv udsendelse om vitaminer o.lign. -Så ville der altid være en opponent, som fik det sidste ord.
-Claus
?
Kærlig hilsen
Henrik Rosenø, M.Sc (civilingeniør)
This post is available in:
![]() Dansk
Dansk